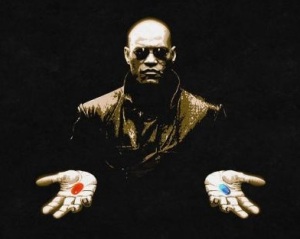
“I know exactly what you mean. Let me tell you why you’re here. You’re here because you know something. What you know, you can’t explain. But you feel it. You felt it your entire life. That there’s something wrong with the world. You don’t know what it is, but it’s there. Like a splinter in your mind — driving you mad. It is this feeling that has brought you to me. Do you know what I’m talking about? Continue reading
Author Archives: adamgordon1978
Healthcare for UK care home residents is broken. How should we go about fixing it?
Adam Gordon is a Consultant and Honorary Associate Professor in Medicine of Older People based in Nottingham, UK. He also edits this blog.
A lot of excellent practice takes place in care homes. This is contrary to the image portrayed in the lay media, where there seems to be near-universal agreement that long-term care in the UK is “broken”. The same media reveals less agreement about what aspects of long-term care, precisely, are broken. Conversely, there is no shortage of suggestions about how one might go about fixing it.
Often overlooked in these discussions is the fact that healthcare provision to care home residents is the responsibility of the National Health Service.
Failure to meet the healthcare needs of residents must therefore reflect, to some extent, on the NHS and how it organises care for them.
The Future Hospital Commission: future-proof doctors need training in geriatric medicine
Dr Adam Gordon is a Consultant and Honorary Associate Professor in Medicine of Older People at Nottingham University Hospitals NHS Trust. He is Deputy Honorary Secretary of the British Geriatrics Society and also edits this blog.

The report of the Future Hospital Commission, published last week, suggested we needed “a cadre of doctors with the knowledge and expertise necessary to diagnose, manage and coordinate continuing care for the increasing number of patients with multiple and complex conditions. This includes the expertise to manage older patients with frailty and dementia.”
The most evidence-based way to manage frail older people is Comprehensive Geriatric Assessment (CGA). CGA has consistently been shown in large meta-analyses and systematic reviews over the last 20 years to improve outcomes for older patients. These include – but are not limited to – decreased risk of cognitive decline and death, increased likelihood of functional independence and a lower probability of readmission to hospital.
Doctors don’t “do” CGA – it is delivered by a multidisciplinary team (MDT). It requires assessment across multiple domains (medical, psychological, environmental, social and functional), accompanied by case management and iteration of management plans. The role of doctors is to provide diagnosis and prognosis, to initiate medical treatments where necessary and to do so with consideration to the broader management plan agreed with the MDT.
If doctors are to do this they need first to understand how CGA works. Continue reading
The future of hospitals is age-attuned
Prof Paul Knight is President of the BGS and is Director of Medical Education and Consultant Physician at the Royal Infirmary, Glasgow.

The Future Hospital Commission (FHC) has published its report and recommendations for ensuring that hospitals are designed around the needs of patients. The report recognises that older, frail and more complex patients with multiple long term conditions are the main patient group cared for in modern hospitals. It is critical that we meet the needs of these vulnerable individuals.
The FHC places welcome emphasis on the importance of Comprehensive Geriatric Assessment (CGA) but at the same time there are significant workforce implications for the expanded use of CGA in general hospitals.
The Vulnerable Older People’s Plan – Important points from the coalface
Dr Adam Gordon is a Consultant Geriatrician and Honorary Associate Professor in Medicine of Older People at Nottingham University Hospitals NHS Trust. He is Deputy Honorary Secretary of the British Geriatrics Society and also edits this blog.
The list of imperatives to improve care for older people is convincing. It’s now difficult to accept a future version of our National Health Service that doesn’t have a coordinated plan for frail older people at its middle. In this respect it’s good to see that the government is taking the issue seriously with a national consultation on it’s Vulnerable Older People’s plan (VOPP). On September 11th, I went to a meeting in London to present the British Geriatrics Society’s position. Continue reading
Your speciality needs you…..to write questions for the MRCP(UK)
Adam Gordon is a Consultant and Honorary Associate Professor in Medicine of Older People based in Nottingham, UK. He is also the editor of this blog.
Good CPD can be hard to come by. Sure, there are endless opportunities to attend symposia and conferences and workshops and away-days……but how often do you engage in a piece of CPD that makes you reflect critically on your understanding of key aspects of your work as a geriatrician, or that makes you question the essence of what it is that separates your specialty from the others, or what makes geriatrics relevant to patient care?
If you’re looking for something more than powerpoint presentations in glamourous venues with finger-food of varying quality, something that encourages you to think deeply and reflect on what it is that is most important about being a geriatrician, then I may have just the thing for you. Continue reading
Closing acute hospital beds for older people – the way to save our services?
Prof David Oliver is a Consultant Geriatrician in Berkshire and a visiting Professor in Medicine of Older People at City University, London. He is President Elect of the British Geriatrics Society.
At the recent King’s Fund Integrated Care Summit, I shared a speaking platform with David Prior – the new Chair of the Care Quality Commission and a man of experience and sincere commitment to improving patient care. In the course of his talk, he stated that “far too many patients are arriving at hospitals as emergencies, with accident and emergency departments out of control and unsustainable in many parts of the country.” He added that “the healthcare system is on the brink of collapse” and “if we don’t start closing acute beds and investing instead in community care, the system will fall over”. He stated that with “almost half of hospitals providing care which is either poor or not terribly good, the pressure means that regulators cannot guarantee there will never be another care disaster such as Mid Staffs”. Continue reading
Health in care homes: can we do better?
Dr Adam Gordon is a Consultant and Honorary Associate Professor in Medicine of Older People at Nottingham University Hospitals NHS Trust and the University of Nottingham. He also edits this blog.
Arrangements to provide health care to UK care homes are often inadequate. In the British Geriatrics Society’s Failing the Frail Report, based on a national survey by the Care Quality Commission, 57% of residents were reported as being unable to access all health care services required. In 2011, a collaboration of health care groups led by the British Geriatrics Society published Quest for Quality, which went so far as to describe existing arrangements as “a betrayal of older people, an infringement of their human rights and unacceptable in a civilised society”.
So, can we do better?
Since 2008, the Medical Crises in Older People (MCOP) research programme at the University of Nottingham has been working to better understand the challenges and opportunities that society faces in providing effective healthcare to care home residents. As this work draws to a close, we are hosting a conference entitled “Health in care homes: can we do better?” in Nottingham on June 14th, 2013. Details of the conference can be found here.
Time to catch up: dementia, medical education and 21st-century healthcare
Dr Ellen Tullo is a Teaching and Research Fellow at the Biomedical Research Centre in Ageing at the University of Newcastle, UK. Her particular area of interest is in how we teach about dementia in order to improve outcomes for patients.
In centuries past, medical students in the UK studied rheumatic fever, smallpox and syphilis as a reflection of the needs of the community that they served. However medical advances and demographic change mean that health and social care professionals now face new challenges and opportunities. Many of these are related to ageing and the need to provide the best possible care to an increasing number of increasingly complex frail older patients. In this context, dementia is an area of current – and growing – importance.
Over the last decade, multiple national audits, reports and policy statements highlighted concerns about the care afforded to people with dementia in both primary and secondary care. The recurrent message from these documents was that education and training about dementia for health and social care professionals must improve.
Moreover, just in the last few weeks , the government’s response to the Francis report reiterated the importance of the issue by affirming their commitment to improving dementia-related training for professionals. So the past decade of auditing, reporting and policy stating does not seem to have prompted the necessary change.
How should we take things forward?
Inside Out of Mind – Exploring Dementia Care through Drama
Professor Justine Schneider is Professor of Mental Health and Social Care at the University of Nottingham, UK. She writes here about an inspirational project which used research outputs to develop a play providing unique insights into dementia care.
Inside Out of Mind is an innovative theatre project which has brought together ethnographic researchers with arts practitioners to tackle the challenge of dementia care. The resulting play brilliantly illustrates the multiple realities of life on a dementia ward, and is an inspiring collaboration between Meeting Ground Theatre Company, Lakeside Arts Centre, The University of Nottingham’s Institute of Mental Health and the NHS.
Inside Out of Mind is based on field notes kept during months of participant observation in dementia wards by researchers Simon Bailey, Kezia Scales and Joanne Lloyd. Writer and Director Tanya Myers used the highly detailed and extensive notes as a “seed” to inspire this play about the largely mysterious world of inpatient dementia care.