“I know exactly what you mean. Let me tell you why you’re here. You’re here because you know something. What you know, you can’t explain. But you feel it. You felt it your entire life. That there’s something wrong with the world. You don’t know what it is, but it’s there. Like a splinter in your mind — driving you mad. It is this feeling that has brought you to me. Do you know what I’m talking about? You can see it when you look out your window, or when you turn on your television. You can feel it when you go to work, or when go to church or when you pay your taxes. It is the world that has been pulled over your eyes to blind you from the truth.
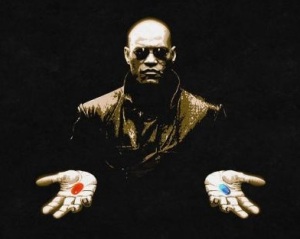
(In his left hand, he shows a blue pill.)
You take the blue pill and the story ends. You wake in your bed and believe whatever you want to believe.
(A red pill is shown in his other hand)
You take the red pill and you stay in Wonderland and I show you how deep the rabbit-hole goes.”
Excerpt from “The Matrix” by Larry and Andy Wachowski
I sat in a meeting recently where very experienced physicians of multiple denominations told me that the most common presentations to hospital were clearly defined syndromes like chest pain and stroke, and that “everybody did geriatric medicine” because the majority of patients presenting to receiving units are old. This, unfortunately, is the world that has been pulled over their eyes, a world reverse-engineered to fit an excessively medicalised model of healthcare focussed around diagnostics.
The reality is, of course, different. The most common presentation is non-specific. Older people – and it is they who comprise the bulk of the acute medical take – most frequently come in with “non-specific functional decline”, “off-legs”, “acopia”, “worsening confusion”. When they do present with specific symptoms such as chest pain, breathlessness, focal neurology, the underpinning reason is not always the most obvious one.
Just “seeing old people” does not make you a geriatrician. Geriatricians do things differently. We start from the patients’ problems and work forward. We understand that, whilst medical diagnosis is essential for effective management, it is not sufficient. We have recognised that frail older patients’ problems are frequently explained by the transection of medical, psychological, functional, social and environmental issues and that these can only be tackled through concerted efforts by a multidisciplinary team. We have, with our colleagues in nursing and the allied health professions, researched how best to assess and support complex, frail older patients and have established a robust evidence base for comprehensive geriatric assessment.
Mary Tinetti challenged our assumptions about the world as it really is when she wrote her article on the end of the disease era in 2004 and her observations are as pertinent today as then.
Being a geriatrician can be tough. Working with complex problems across multiple domains is intellectually challenging, as is working with multiple colleagues, from multiple disciplines, in environments ranging from community-based intermediate care to the acute hospital. Dealing with adaptive rehabilitation, where aspirations are often dashed, can be dispiriting and there’s more than the fair dash of death and dying. A lot of our patients present during the acute take and so there’s a lifetime of obligation to acute hospitals to consider.
Junior doctors sometimes struggle, therefore, to see why to choose geriatric medicine. My response is to offer them the red pill, to show them the world as it really is and the things that can be achieved when you recognize the types of problems that older people really have and adopt an appropriate, multidisciplinary, iterative response where diagnosis is key – but not the be-all-and-end-all. The alternative is to go back to bed and believe what you want to believe.

There are more than two colour options – I’d choose purple and not just because Cadbury’s couldn’t brand it or that it identified with the important novel but for its alleged affinity to passion etc.
No no no no no no no! Review the need for the red pill, discuss with with the patient and, if appropriate, their family, and then decide to stop the red pill, and the blue, white, and green ones. And involve the MDT.